Formulation and evaluation of transdermal patch of Aceclofenac
Keywords:
Aceclofenac, Transdermal Film, Permeation enhancer, In-vitro permeation studyAbstract
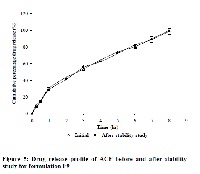
The purpose of this research was to develop a matrix-type transdermal therapeutic system containing drug Aceclofenac with different ratios of hydrophilic (hydroxyl propyl cellulose) and hydrophobic (ethyl cellulose) polymeric systems by the solvent evaporation technique by using 15 % w/w of dibutyl phthalate to the polymer weight, incorporated as plasticizer. Different concentrations of oleic acid and isopropyl myristate were used to enhance the transdermal permeation of Aceclofenac. The physicochemical compatibility of the drug and the polymers studied by differential scanning calorimetry and infrared spectroscopy suggested absence of any incompatibility. Formulated transdermal films were physically evaluated with regard to thickness, weight variation, drug content, flatness, tensile strength, folding endurance, percentage of moisture content and water vapour transmission rate. All prepared formulations indicated good physical stability. In-vitro permeation studies of formulations were performed by using Franz diffusion cells. Formulation prepared with hydrophilic polymer containing permeation enhancer showed best in-vitro skin permeation through rat skin (Wistar albino rat) as compared to all other formulations. The results followed the release profile of Aceclofenac followed mixed zero-order and first-order kinetics in different formulation. However, the release profile of the optimized formulation F9 (r2 = 0.9935 for Higuchi) indicated that the permeation of the drug from the patches was governed by a diffusion mechanism. Formulation F9 showed highest flux among all the formulations and 1.369 fold enhancements in drug permeation. These results indicate that the formulation containing 15 % of oleic acid with 10 % Isopropyl myristate give better penetration of Aceclofenac through rat skin.
References
Misra AN. Controlled and Novel Drug Delivery. In: N.K. Jain(Eds.), Transdermal Drug Delivery New Delhi, India: CBS Publisher and Distributor. 1997. 100-101.
Chien YW Transdermal therapeutic system. In: Robinson, JR, Lee VHL., eds. Controlled Drug Delivery Fundamentals and Applications 2nd ed. New York: Marcel Dekker, Inc. 1987; 524-552.
Keith AD. Polymer matrix consideration for transdermal devices. Drug Dev Ind. 1983.;9: 605-621.
FitzGerald GA, & Patrono, C. The coxibs, selective inhibitors of cyclooxygenase-2. N Engl J Med. 2001;345(6):433-42.
Laurent B, Annette M, Jean-Pierre D Daniel-Henri M. Effects of diclofenac, aceclofenac and meloxicam on the metabolism of proteoglycans and hyaluronan in osteoarthritic human cartilage. Br J Pharmacol 2000;131: 1413-1421.
Hinz B, Rau T, Auge D, Werner U, Ramer R, Rietbrock S, Brune K. Aceclofenac spares cyclooxygenase 1 as a result of limited but sustained biotransformation to diclofenac. Clin Pharmacol Ther. 2003; 74(3): 222 - 35.
Cohen EM, Grim WM, Harwood RJ, Mehta GN. Solid state ophthalmic medication. United States Patent No. 1979; 4:179,497.
Harwood RJ, Schwartz JB. Drug release from compression molded films: preliminary studies with pilocarpine. Drug. Dev. Ind. Pharm. 1982;8:663 – 682.
Dumortier G, Zuber M, Chast F. Systemic absorption of morphine after ocular administration: evaluation of morphine salt insert in vitro and in vivo. Int. J. Pharm. 1990;59: 1–7.
Kusum DV, Saisivam S, Maria GR, Deepti PU. Design and evaluation of matrix diffusion controlled transdermal patches of verapamil hydrochloride, Drug Dev. Ind. Pharm. 2003;29:495–503.
Limpongsa E, Umprayn K. Preparation and evaluation of diltiazem hydrochloride diffusion-controlled transdermal delivery system. AAPS PharmSciTech. 2008;9(2):464-70
Sakellariou P, Rowe RC, White EFT. An evaluation of the interaction and plasticizing efficiency of the polyethylene glycols in ethyl cellulose and hydroxypropyl methylcellulose films using the torsional braid pendulum. Int. J.Pharm.1986;31:55–64.
Cooper ER. Increased skin permeability for lipophilic molecules. Pharm Sri. 1984;73:1153-1156.
Goodman M, Barry BW. Lipid-protein-partitioning (LPP) theory of skin enhancer activity: finite dose technique. Int J Pharm. 1989; 57:29-40.
Hu JH, Zhu Y. Effect of enhancers on the permeation of ketoprofen in-vitro. Yao-Hsueh-Hsueh-Pao. 1996; 31:48-53.
Chi SC, Park ES, Kim H. Effect of penetration enhancers on flurbiprofen permeation though rat skin. Int. J. Pharm. 1995;126:267-274.
Kim DD, Chien YW. Transdermal delivery of dideoxynucleoside-type anti-HIV drugs. 2. The effect of vehicle and enhancer on skin permeation. J. Pharm. Sci. 1996; 85:214-219.
Arora P, Mukherjee P. Design, development, physicochemical, and in-vitro and in-vivo evaluation of transdermal patches containing diclofenac diethylammonium salt. J Pharm Sci. 2002; 91: 2076-2089.
Amnuaikit C, Ikeuchi I, Ogawara K, Higaki K, Kimura T. Skin permeation of propranolol from polymeric film containing terpene enhancers for transdermal use, Int. J. Pharm. 2005; 289:167–178.
Verma PRP, Iyer SS. Transdermal delivery of propranolol using mixed grades of Eudragit: design and in-vitro and in vivo evaluation. Drug Dev. Ind. Pharm. 2000;26: 471–476.
Devi VK, Saisivam S, Maria GR, Deepti PU. Design and evaluation of matrix diffusion controlled transdermal patches of verapamil hydrochloride, Drug Dev. Ind. Pharm.2003; 29:495–503.
Gupta R, Mukherjee B. Development and in-vitro evaluation of diltiazem hydrochloride transdermal patches based on povidone-ethyl cellulose matrices. Drug Dev Ind Pharm. 2003; 29:1 – 7.
Krishna R, Pandit JK. Transdermal delivery of propranolol, Drug Dev. Ind. Pharm. 1994 ; 20:2459–2465.
Julraht K, Keith AP, James AW. Development of a Transdermal Delivery Device for Melotoin In-vitro Study. Drug Dev. Ind. Pharm. 1995; 21:1377–1387.
Ho HO, Chen LC, Lin HM, Sheu MT. Penetration Enhancement by Menthol Combined with a Solubilization Effect in a Solvent System. J. Control. Release, 1998; 51: 301–311.
Yamune M, Williams A, Barry B. Terpenes Penetration Enhancers in Propylene Glycol/Water Co-solvent Systems: Effectiveness and Mechanism of Action. J. Pharm. Pharmacol. 1995; 47: 978–989.
Williams, A., & Barry, B. Terpenes and the Lipid–Protein Partitioning Theory of Skin Penetration Enhancement. Pharm. Res. 1991; 8: 17–24.